Book Appointment
Fillup the form to make an appointment with the doctor
Trigger thumb is a common disorder noticed in pediatric orthopedic practice. It is occasionally seen in the first six months of life and is usually noticed when the child starts to grasp objects or reaches out for objects.
Clinical Feature Inability to extend the IP joint of the thumb and held in flexion as shown in the picture. Occasional triggering and straightening out of thumb and difficulty to bend it
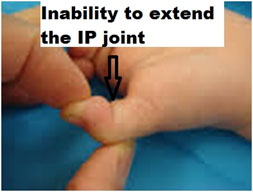

If the child is less than nine months of age, then stretching exercises can be taught to the parents to straighten the IP Joint, and if the presentation is after the age of One year, then a surgical release of the A1 pulley at the 1st MCP joint is done.
Calcaneovalgus foot is a common deformity that appears at birth. This deformity consists of the dorsum of the foot being near the shin and difficulty to plantarflex the foot. In the extreme form, the dorsum of the foot might touch the shin. This is mainly due to intra-uterine positioning of the foot, and the tendency is that the deformity will correct itself over a period of time. Its importance lies in making the differentiation with more difficult surgical problems. It can be associated with a posteromedial bowing of the tibia, which is a benign condition. Treatment is usually observation and manipulation some times. The primary differential diagnosis is “Congenital Vertical Talus or Oblique talus deformity.”
Most CTEV patients have to be referred at birth for further management as delay in presentation makes correction of the deformity a little complicated.
Points to counsel before referral-
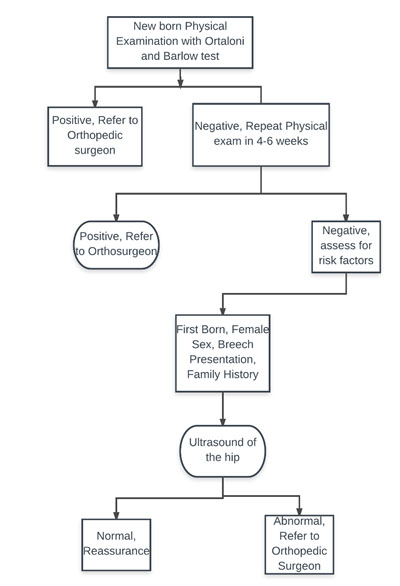
Approach to the referral of DDH patient
POINTS TO PONDER ABOUT HIP ULTRASOUND
Posteromedial bowing is a benign clinical condition with a good natural history. It is mostly due to the intrauterine positioning of the leg. It is most often associated with calcaneovalgus foot. It spontaneously corrects by the age of 5-7 years. If there is more than 3-4 cm of shortening, then surgical intervention is necessary to equalize the limb length.
Most often than not, this should not be confused with anterolateral bowing of the leg, which is almost always pathological. Anterolateral bowing is mostly because of congenital pseudarthrosis of the tibia. Congenital Pseudarthrosis of tibia and fibula is one of the most challenging surgical problems in pediatric orthopedic surgery, and it is important to distinguish from benign posteromedial bowing of the tibia.
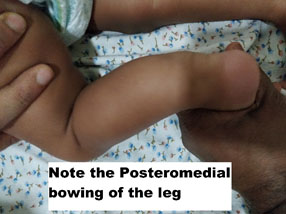
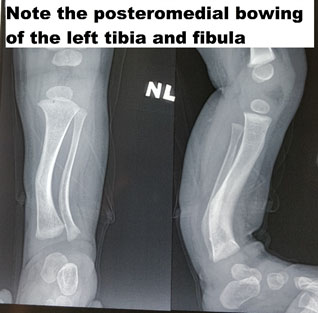
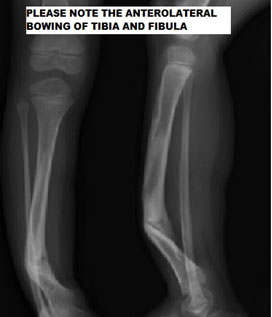
It is important to refer all bowing of the leg to the pediatric orthopedic surgeon as sometimes it is difficult to differentiate the two disorders. If one is very sure about the Posteromedial bowing of the leg, then one can wait for 2-3 years with reassurance to the family
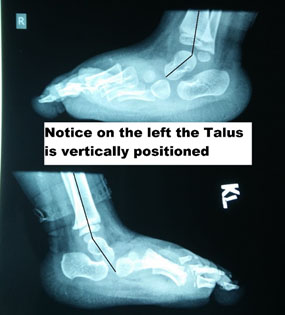
CVT is a deformity where there is equinus of the hindfoot and dorsiflexion of the forefoot. The fundamental point of note is the “tightness” of the tissues. This deformity has been called as “rocker bottom foot” or “Persian foot.” It is a very rigid deformity and is almost always a disorder that requires either manipulation or surgical treatment. The difference between the positional calcaneovalgus and CVT is the stiffness in this condition. There is an intermediate entity, which is “Oblique talus,” where there is dorsal displacement of Navicular on the talar head but is still reducible on the talus in plantar flexion. It warrants immediate referral to an orthopedic surgeon and needs a surgical solution. It is usually associated with syndromes like arthrogryposis or myelomeningocele.
A lateral X-ray of the foot will clearly show that the talus is in a vertical position, whereas the relationship in the flexible deformity is anatomical.
The deformities in the pediatric age group could be-
Rotational deformities of the lower extremity are intoeing mainly due to increased femoral neck anteversion, Internal tibial torsion or metatarsus adductus.
There are large number of parents who are concerned that the baby is unable to “straighten” out the legs. This might be a cause of parental anxiety and frequent visit to the pediatrician. Given the intra-uterine positioning of the baby, it is not unusual for a newborn to have a 30-60 degree flexion at the hip joint and 25-40 degree flexion at the knee joint till about three months of age. They also have an external rotation contracture positioning at the hip joint, which might last until nine months of age.
INTOEING
Intoeing is mainly due to a combination or individually of three clinical entities, Metatarsus Adductus, Internal Tibial Torsion & Increased femoral neck ante-version. This is one of the common concerns for which patients are referred to a pediatric orthopedic surgeon, and mostly due to social pressure and comments, parents want the deformity assessed and usually pressurize the treating doctor for “some treatment.”
MA is a deformity where the big toe points towards the midline due to tightness in the Abductor Hallucis muscle. It has also been called “monkey toes” as it is seen in apes. MA is a self-limiting disorder which needs only reassurance. Usually, rather than presenting as a deformity with only the big toe pointing inwards, it is part of more significant deformity, which is referred to as “Metatarsus adductovarus” which means that along with big toe pointing towards the midline the sole also looks inwards. This condition is commoner than the isolated “adductus” deformity. It is commonly noticed up to 24 months after which there is a tendency for automatic correction.
Assessment of this deformity consists of pushing the ball of the big toe laterally to see if it crosses the midline and if it does not reach the midline or cross it, then we offer treatment for babies 3-6 months of age. The procedure will consist of serial casting, Adaptive shoes, and braces till two years of age but usually individualized as per patient requirement.

ITT is a deformity that is commonly seen in the age group of 6-24 months, and it usually resolves, as the child grows older. ITT usually presents as “in-toeing” and clumsy gait. This is primarily a clinical diagnosis. The best way to diagnose the tibial torsion is to look at a child in the seated position with the tibial tuberosity pointing forward then comparing the trans-malleolar axis (Line connecting the medial and lateral malleolus). A simpler method is looking at the second toe and comparing the position of the tibial tuberosity with the second toe position. Having the child lie prone on its abdomen and looking at the thigh and foot angle would also give an idea about internal tibial torsion. Usually, any associated deformity of the foot does influence the position of the second toe in comparison with the trans-malleolar axis. Thus, we always recommend the trans-malleolar axis for the assessment of tibial torsion. The natural history of this disorder is such that it almost always resolves spontaneously, and very rarely does it need surgical correction. Various braces were used in the past; presently, there is no recommendation for bracing. Very infrequently would surgery, which consists of a de-rotation osteotomy of the distal tibia done in symptomatic kids.
FNA is a condition where the intoeing is because of excessive forward pointing of the neck of the femur with respect to the knee joint line (the angle formed between the coronal plane and the neck of femur is called as ante-version. Most often, this condition presents in kids between 2-8 years of age and is equal in both the sexes. It manifests as excessive inward-pointing of the toes, especially when the child is tired, running. Parent’s complaint that the child sits in W position or reverse tailor position. The best way to examine this is to put the child prone and measure the amount of internal rotation (IR) and compare it to the opposite hip. In a prone patient, hip rotation outside is an internal rotation of the hip, and the reverse direction is External rotation.

WHEN TO REFER
Angular deformities are another essential topic of parental concern. There is a varying and changing pattern of angular deformity, which happens in the knee joint that it is a frequent source of anxiety to parents. Typically a newborn would have bow legs which drifts into valgus by the age of two years and reaches maximum valgus by the age of 7 years and then stabilizes to a mild physiological valgus by early teen ages, which is depicted well in the graph below.
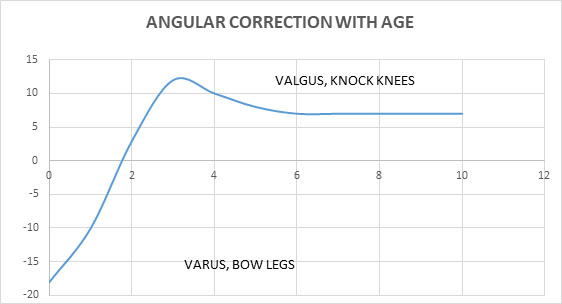
The important point of note is to examine the fingerbreadth distance between the two knees in bow legs and the trans-malleolar distance in knock knees. A vast majority of kids have physiological bowing and are referred more for reassurance than intervention to a pediatric Orthopedist. But, the critical point to remember is that there is a small subset of patients who could have an underlying metabolic disorder that needs to be diagnosed and treated appropriately. The differential diagnosis is rickets, traumatic, or infective growth plate insults, dysplasia, Blount’s disease, and neoplasms. It is essential to investigate adequately if there is associated systemic features, asymmetric presentation. There was a tendency in the past to treat these disease with braces, manipulation and various other intervention but ultimately studies have found that it does not make much difference
Linear Deformity
Limb length discrepancy (LLD) is widely seen in society. About 30% of adults have 1-2 cm difference in their lower limb length. Minor variations in limb length are not causes of worry and can be left alone. The problem is when the deformity leads to functional disability in the child.
Causes-
Any child with a limp should be evaluated for limb length discrepancy and should be assessed clinically by measurement of limb length. Techniques of measurement were by using blocks below the foot and using tape measurements. Radiologically, hip, knee, and ankle scanograms help us to assess the same and get objective measures.
TREATMENT


Recurvatum is a spectrum disorder where it could be due to mal-positioning in utero or could be part of a genetic spectrum.
Pathology-
There is tightness in the quadriceps tendon, with anterior subluxation of the hamstring tendons. The collateral ligaments are tight as well.
IMPORTANT ASSOCIATION
DDH- about 50% of patients have DDH, and the child needs to be examined for DDH
Associated syndromes- Larsen, Myelomeningocele, and Arthrogryposis
Clinical Findings and Treatment
The deformity is visually apparent and is noticed at birth. Treatment usually consists of serial plaster casting and once knee joint reduced, Pavlik Harness for treatment of the associated DDH
Late Presentation
If a child presents late, then the child has to be treated operatively by soft tissue release and open reduction of the knee joint.
Immediately at birth
Rule out associated deformity esp. DDH



FFD is a deformity where there is anterior convex bowing of the knee joint. This could be caused for various reasons which include-
Trauma
Cerebral Palsy
Infection
Prolonged immobilization
Congenital abnormality
The clinical findings in this situation are inability or difficulty for the patient to walk. There will be a gross limb length difference leading to severe functional impairment. Many times, these patients are confined to wheelchair, and that leads to further contractures.
Treatment of this condition depends on the underlying cause and status of the knee joint. Growth modulation surgery is offered if there is a growth plate abnormality. If there is arthritis of the knee joint, then arthritis treatment might have to be combined with deformity correction.
Symptomatic deformity (pain, swelling inflammation)
Functional deficit
Long-standing symptoms
If congenital immediate- to rule out septic arthritis of the knee joint
CASE 1
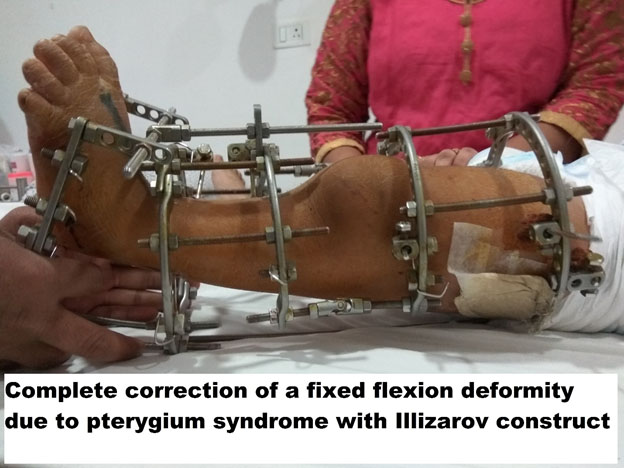
Post-traumatic with surgical fixation leading to a 60-degree flexion deformity in a 30-year-old female patient who was walking with difficulty. After six weeks of distraction, please note the achievement of full extension.




Case 2
A 10-year-old boy who presented with Fixed flexion deformity of the knee, had repeated failed surgeries (2 number) as part of a complex pterygium syndrome and difficulty in gait.
Cerebral palsy patients have many needs, and pediatricians are intimately involved in their care. No other branch of medicine exemplifies the difficulty and challenges of multi-disciplinary care than cerebral palsy. Pediatricians, as final arbitrators of care and decisions, must consider the cost factor when they refer patients for subspecialty care. CP families might not have the resources to spend on Physical Therapy (PT), Occupational Therapy (OT), and special needs school. The stress of family on mobility will sometime take away the more critical need to ensure skills training in these children. Thus the child must be referred to PT and Orthopedic surgeon, but also the family should be instructed to spend more energy on ensuring the child gets life skills.
There are various scoring systems designed in CP, but the most used and enduring has been the GMFCS grading (Gross Motor Function Classification System). It is a simple, useful classification helpful in communication as well as treatment planning with five grading system
Type 1 – walks without functional limitation
Type2 – Walks with functional limitation
Type3 – Walks with a handheld mobility aid
Type4 – Limited labored mobility with aids and needs motorized assistance for distances
Type5 – Wheelchair bound
| AGE | MOBILE ( GMFCS I-III) | NON-AMBULATORY (IV-V) |
|---|---|---|
| 0-5 Years | Spasticity management Orthotics | Spasticity management
Orthotics
Hip Surveillance |
| 6-18 | SEMLS ( Single Event Multi-Level Surgery) | Quality of life Management |
A cerebral palsy patient should have had neurology, Physical therapy from a qualified pediatric PT, and Occupational therapy before being seen by a pediatric orthopedic surgeon. The role of stretching cannot be emphasized more during counseling