Book Appointment
Fillup the form to make an appointment with the doctor
Hip Problems Total Hip Replacement
The hip is a ball and socket joint where the smooth head of the femur moves in the socket piece, which is the acetabulum in the pelvis. This ball and socket arrangement facilitates a smooth movement and ability to take the pressure and walk for long distances
Indications for hip replacement
Arthritis
AVN of the hip
Rheumatoid arthritis
Trauma

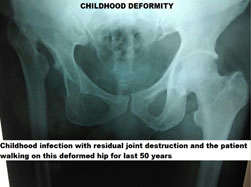
Considering each of these indications, for poorly understood reasons, primary osteoarthritis (OA) is relatively uncommon in Asians in comparison to Caucasians (American and European population). Thus the need for knee replacement is much higher in India in contrast to a hip replacement
The most common reason THR is done in India is for secondary degenerative arthritis due to AVN (Avascular Necrosis) of the hip. Where the bone collapses and leads to osteoarthritis of the hip. The other causes like the neck of femur fracture can also be an indication for THA.
The human hip joint is a ball and socket arrangement where the ball is on the side of the thigh bone, and the socket piece is called the acetabulum. They are extremely congruent so that there is pain-free movement between both the smooth surfaces, and we can move freely. Unfortunately, if there is damage to that extremely smooth surface (the lining is called cartilage), then the patient develops pain. The treatment for which is to replace that worn-out surface with artificial components and is called as hip replacement.
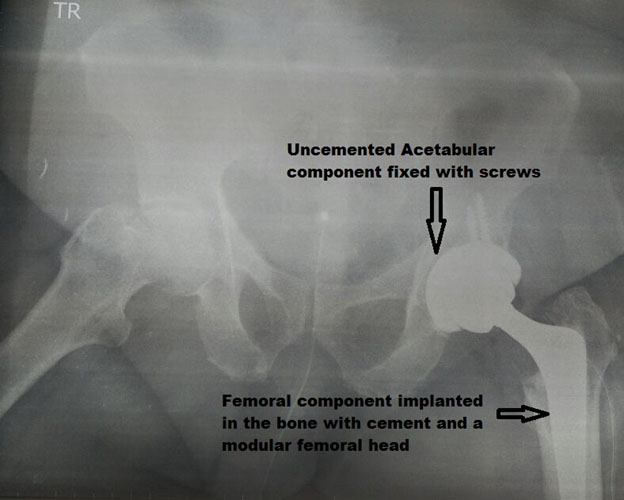
The hip replacement consists of replacing the acetabular side with either the metallic or plastic component and the femoral side with a metallic stem articulating with each other with a circular bearing surface.
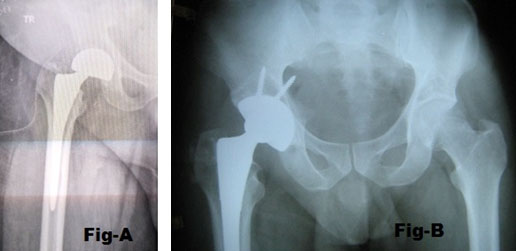
Hip replacement can be broadly classified as partial and total hip replacement. Partial hip replacement is called as “Hemiarthroplasty,” and full hip replacement is “Total Hip Arthroplasty (THA).” The fundamental difference is in the acetabular socket piece wherein Hemiarthroplasty (Fig-A) there is metal against cartilage as the bearing surface while in THA it artificial bearing surfaces on either side (Fig-B).
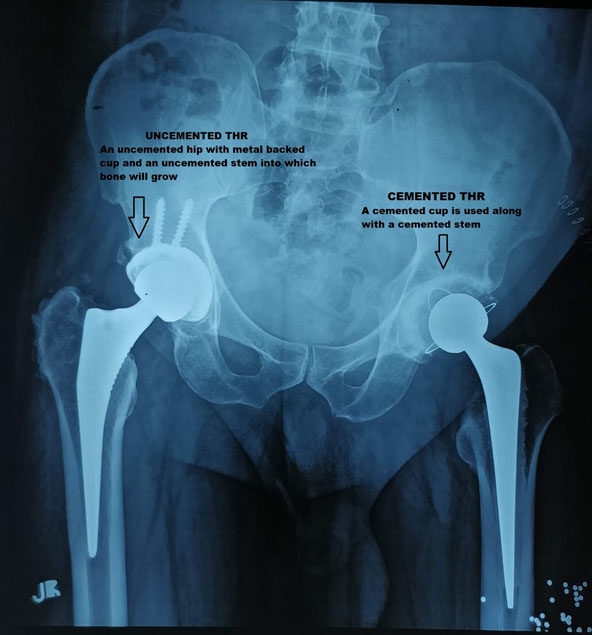
Based on the type of fixation of the metal onto the bone, the THA prosthesis are divided into cemented, Uncemented THA &Hybrid THA.
Cemented THA is a design that started in the 1960s with the original designer of THA named Dr. John Charnley. The metallic component of the prosthesis is fixed to the bone with a filling agent called “Bone Cement”. Bone cement’s chemical composition is “PMMA- Poly Methyl Metha Acrylate.” The acetabular component (Plastic liner) is cemented directly into the acetabulum. The longest follow up for any stem design, and excellent survivorship has been of a design called “Exeter hip,” where the metallic component is seated inside the thigh bone with bone cement.
Bone cement is a very versatile thermoplastic whose chemical name is “polymethyl metha acrylate”. PMMA has a wide industrial application for its versatility. In modern medicine, PMMA is used in the lens for the eye and filling agent in joint replacement surgery. Bone cement works like a filler and not a binder. It fills all the crevices of bone and rough metal, thereby rendering it resistant to an extraordinary amount of compression forces.
It is a joint replacement where both the acetabular side (the cup side) and the head of the femur (the ball side) are replaced with artificial components into which bone will grow. The underlying belief is that once the bone has grown directly into the prosthesis, then effectively, it should last much longer than the older generation of implants. Though the longevity of hip replacement prosthesis has been excellent of about 90 % survivorship at 15-20 years, it is still not perfect.
Cemented Vs. Uncemented has been a point of vigorous debate amongst joint replacement surgeons. The proponent of cemented hip replacement would argue that it is much cheaper. The survivorship of both cemented femoral and acetabular components are better. The chances of breaking the femur are much lower while performing the hip replacement.
The proponents of uncemented would argue that the present generation of the prosthesis has been designed in such a way that they should last much longer than the previous designs. It would avoid the medical problems while inserting cemented components, which could sometimes lead to a concerning amount of low blood pressure, fat embolism.

There is a definitive role for both types of devices based on the patient’s medical condition, affordability, and anatomy. It could be tailored based both on medical as well as social reason with absolutely no compromise in the ultimate functional outcome for the patient.
The early total hip replacement was all stainless steel stem design as it was a cemented stem and was generally highly polished. Later on, the un-cemented stem design was incorporated with the idea that bone could grow into the metal. Thereby the roughening of the stem started, and currently, titanium is the best metal where bone grows into. Thus the present un-cemented stems are mainly titanium except in the crown or the head where the weight resistance of titanium is weak and therefore has been changed to cobalt chrome.

“Bearing surface” means the exact articulation where the movement will occur. There have been various designs and bearing surfaces that have evolved in joint replacement surgery.
Metal on plastic
Ceramic on Ceramic
Ceramic on plastic
Metal on metal
An ideal bearing surface should give a durable, pain-free range of movement with little damage to bone and should provide an extended-lasting function. Presently, there has been a tremendous improvement in bearing surfaces and some of which will last for decades. But, there is no bearing that will last a lifetime for a patient. Each of the bearing combinations has advantages and disadvantages of clinical and financial significance
In THR, the most common bearing surface is metal on polyethylene. The polyethylene is nothing but a high-grade plastic whose material properties are improved recently by a technique called cross-linking. Cross-linking prevents particle loss and, thus, lesser bone damage. The ball of the head is usually cobalt-chrome because it has better properties than titanium to bear weight. The rest of the femoral component is generally titanium, so that bone grows well into the metal. But for femoral head where there is load-bearing, Cobalt chrome behaves better than other combinations. Stainless steel heads are also available to help with bearing weight and can be an acceptable alternative, especially because of their cost-effectiveness.
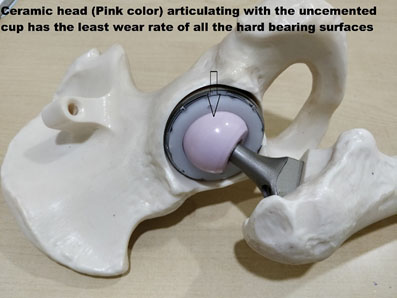
Ceramic is a hard material that is widely used as a bearing surface. It has excellent friction and wear properties but is brittle. The advantage of Ceramic is it causes very minimal wear. Even when coupled with the polyethylene acetabular component, it gives long survivorship. But has a higher chance of fracture and Ceramic on the ceramic bearing surface has known to cause squeaking in 1-6% of patients.
Squeak has been a poorly explained phenomenon that is hard to predict and difficult to treat. It does not impede functions but can be a significant disadvantage for some patients for social reasons.
Metal on metal bearing has been in the news recently for all the wrong reasons. Metal on metal conceptually makes sense and quickly became popular because it was cost-effective and provided the ability to use large diameter heads to reduce the dislocation rates. But, the problem of metal on metal bearing has been the discovery of metallosis and significant metal related complications.
The metallic ions of Cobalt and Chromium are released into the bloodstream, which can cause significant local and general problems. The local issues related to metal ions are ALVAL, ARMD, and Pseudotumor. Each one of these means that the metal particles cause inflammation in the local tissue that leads to destruction and damage to the surrounding tissue. The present safe cut off level in the bloodstream after a joint replacement with MoM bearing is two ng/ml of Cobalt and Chromium. The Systemic side effects (Other than the hip) include hearing defects, Cardiac rhythm disturbances, Visual problems including blindness, rarely some malignancies (cancers).
The problems of MoM have been clearly described in a unique Total Hip Replacement called a surface replacement, which was a rage a couple of years ago. A prosthetic design called ASR was showing signs of early failure and resulted in significant problems of MoM bearings. Also, some used MoM bearings during total hip arthroplasty, which have also shown signs of early failure. It is safe to say that given the alternatives available and the significant complications of metal on metal bearing surface, there is minimal to no role for this bearing surface in the present total hip replacement scenario.
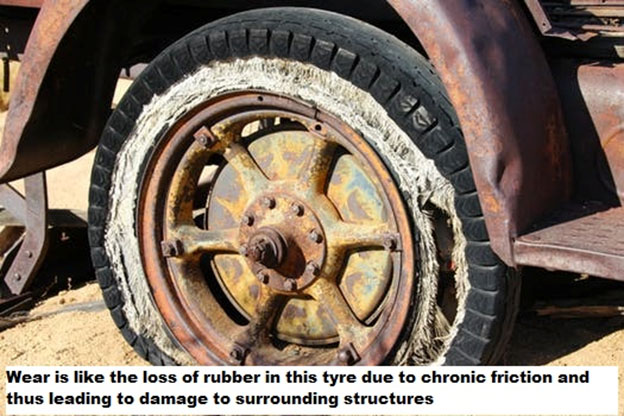
When trying to understand a bearing surface, many patients wonder what is the idea of “Wear”? Simply put, wear is a phenomenon of material degradation when two surfaces rub against each other. In a THR wear esp., the microscopic plastic particles can destroy bone by eliciting an inflammatory response.
The medical team will evaluate medical fitness. Since THR is done in two groups of patients elderly with hip problems or the young adult, the approach will be slightly different. The elderly adult should be evaluated for anemia, cardiac issues, and any correctable illness. While in the young adult, it is crucial esp. in the trauma scenario, to rule out other injuries that might cause a delay in rehabilitation.
Dental problems and urinary infections have to be appropriately managed before an individual undergoes THR to reduce the risk of infection. Obesity has adverse outcomes, and if possible, it is essential to reduce weight pre-surgically.
It is essential to make social adjustments before a THR important ones being appropriate toilet raise, being comfortable with the use of crutches and changes for travel like getting in and out of a car or other modes of transport
Patients should be aware of the risk of dislocation, which is highest in the first 2-3 months after surgery.
To avoid sleeping on the opposite side of the surgery for 6-8 weeks and using a pillow between the legs to prevent legs from crossing over
To avoid sitting cross-legged
To avoid squatting or sitting on the floor
Personal hygiene would need attention and generally should avoid taking a shower in the first week after surgery or should ensure that there is no soakage of dressing.
Stair climbing leading with the non-operated side when going up and using the operated leg first when coming downstairs
Complications after total hip replacement
Dislocation is one of the critical complications that people should be aware of after THR. It happens in 3-4% of patients. The risk factors for dislocation of a hip joint are-
Surgeon related-
1. Faulty component position
2. Improper soft tissue management (esp. after a posterior approach)
3. Incorrect implant selection
Patient-related-
1. Not following postoperative instructions
2. Risky positions of the hip
Disease-related-
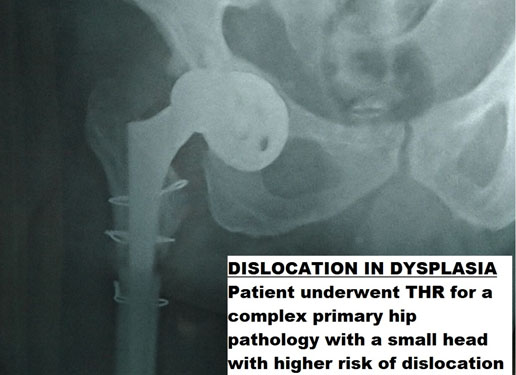
1.THR for hip dysplasia where the cup and head size is generally small
2. For the neck of femur fracture where the soft tissue is not adequately contracted.
The surgeon should pick the appropriate implant, position in the “safe arc of motion,” and perform an excellent soft tissue repair. Patients should follow strict postoperative instructions. Finally, even if a hip is dislocated, it can be closed reduced and made stable by immobilization.
The most dreaded complication after a joint replacement surgery is an infection. If a prosthetic joint esp. hip gets infected, it a surgical nightmare where a diagnosis can be difficult and management complicated. Infection after THR is around 1-2% higher in patients with Rheumatoid arthritis and Diabetes.
Strategies must be employed to avoid prosthetic joint infection. It consists of a structured approach where the patients are optimized for the outcome, operated in an ultraclean operating environment and surgeon performing right technical surgeries
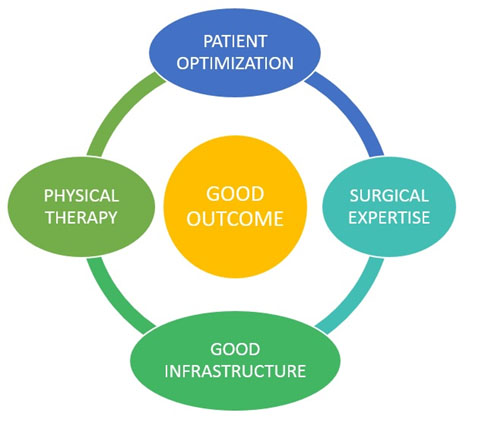
Optimization is a relatively new concept in joint replacement, especially in the Indian context. Presently, patients are evaluated by surgeons and are immediately subjected to a joint replacement, which will significantly undermine the outcome for a hip replacement. An elective surgery like a hip replacement needs proper health optimization so that there can be a promotion of positive outcome after THR
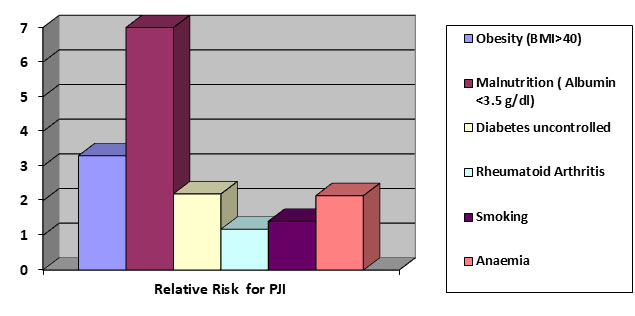
Factors like Hypertension, Diabetes, Renal failure, Cardiac failure, Anemia, Thyroid problems are called co-morbidities, whose presence increases the risk of infection after joint replacement surgery. Therefore it is “absolutely imperative” that the patient’s health is evaluated and optimized where the effect of the co-morbidities is taken care of and thus reduces the risk of complications.
| Co-Morbidity | Co-Morbidity |
|---|---|
| Obesity (BMI>40) | 3.3 |
| Malnutrition ( Albumin <3.5 g/dl) | 7 |
| Diabetes uncontrolled | 2.2 |
| Rheumatoid Arthritis | 1.18 |
| Smoking | 1.41 |
LLE is not an uncommon problem that can occur after joint replacement surgery. If there is a difference of less than 1.5 cm, it is barely noticeable, but an increase in more than this can interfere with functioning and may lead to less patient satisfaction. The surgeon intra-operatively can control the limb length difference by matching the length and appropriate surgical planning. But, in some situations, the surgeon might deliberately increase the length to prevent dislocation. If the difference is <, 2 cm can be managed by shoe raise on the short side.
DVT is a common problem after THR. DVT happens because there is venous pooling, elderly who are not mobile, and THR itself predisposes for DVT. The fundamental way to prevent DVT is to be aware of it and use mechanical methods like compression stockinet, foot pumps after surgery with calf exercises. Your surgeon might prefer to use medications to prevent DVT in the form of Heparin, Warfarin, or aspirin. Postoperative DVT prophylaxis lasts for 4-6 weeks duration.
Swelling is another common problem after THR. Most often, this is a benign problem, which is due to inactivity and inability of the calf pump to push blood against gravity but also could mean DVT. If there is a high index of suspicion, especially if the patient has respiratory symptoms like breathlessness, chest pain, then Doppler scanning is beneficial.
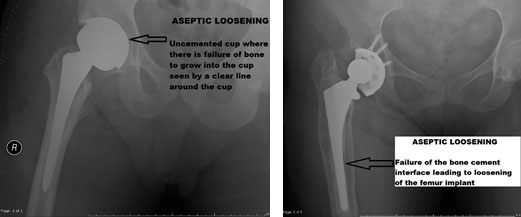
THR implants are designed to help patients function normally for an extended period. But, in some situations, either due to old design or general material fatigue, there could be a failure of implant and bone interface. Patients typically experience start-up pain, which is pain on standing and the first few steps. It could present either with failure of the acetabular side of the femoral side. There could be wear out of the polyethylene bearing surface and lead to complications as well.
Fortunately, nerve weakness after THR is rare. It could happen in nerves in the front of the hip called as femoral nerve or the commoner one in the back named as the sciatic nerve.
The sciatic nerve is the largest nerve of the human body and is located right behind the hip joint. The reported incidence of sciatic nerve palsy ranges from 0.6 to 3.8%. It could be stretched or damaged during certain maneuvers of the hip joint during THR esp. traction for reduction, Improper retractors, or even due to malpositioned components. Sciatic nerve palsies generally recover in 3-4 months, esp. the common peroneal nerve component. The main presentation is foot drop, and the primary stay of management is to apply a foot drop splint and keep the joints supple till recovery happens.
Femoral nerve palsy has been reported in patients esp with direct anterior THR, where the retraction places the femoral nerve at risk. The complication rate is 1 in 500 (0.2%) surgeries, but if it happens leads to significant weakness to walk and a need for assistance device for the patient to walk.