Book Appointment
Fillup the form to make an appointment with the doctor
Total Knee Replacement Techniques Of Total Knee Replacement
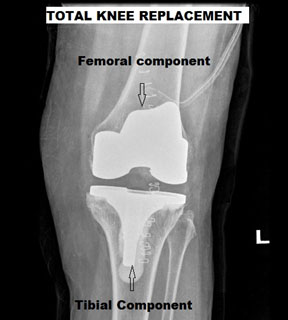
It is essentially replacing the worn-out “bearing surface” of the knee joint by artificial smooth surface of metal and plastic. The cartilage, which is worn out, cannot be regenerated in any objective way in the present scenario, and thereby the only predictable method is to replace it.
The surgery involves an incision in the front of the knee. Cutting the ends of the thigh bone(Femur), the shin bone(tibia), and fixing the metallic components (sometimes the plastic part of the tibia is attached directly to bone without metal there) to the bone with cement which essentially bonds the metal to the bone.
Pain & anesthesia in the management of Total Knee replacement has made tremendous progress. Multimodal analgesia is the order of the day. It means combining different methods of anesthesia- general, regional, and local to obtain optimum pain relief with minimal side effects. These techniques help in the early mobilization of the patient and quicker recovery.
General Anesthesia is a technique where medication is given to induce a deep sleep-like state. The doctor generally secures the airway by passing a tube through the mouth into the trachea (the windpipe). This helps in using anesthetic gases or IV medication to continue to maintain anesthesia, and the patient is completely unaware of the surroundings.
Regional Anesthesia is placing medication around the spinal cord in the lower back where it could be of two types- Spinal and Epidural. Most often than not, your anesthetist will use both techniques to obtain pain relief during the surgery. Spinal for surgical pain and your post-operative pain by medicines given through the epidural catheter. Recently, Pain specialists are placing catheters or just medication around the femoral nerve and sciatic nerve. These nerves carry pain sensation to the brain so that your pain decreases without the side effects of intravenous pain medication.
Informing the surgical team ahead of time will give ample scope to assess which medications to continue in the days before surgery. There are medications like Aspirin, Clopidogrel, High dose vitamins that usually need to be stopped one week before surgery. Pain medications like Voveran, brufen should also be stopped one week before surgery. But, again, all the medicines should be discussed with the surgical team and stopped only after prior instructions by the treating team. Blood thinners may need continuation in certain situations where an individual has recent cardiac stenting done. Avoiding such medications decreases bleeding risk and reduces the need for blood transfusion. Meanwhile, one must continue to take Thyroid, Hypertension, and Diabetes medication right up to the time of surgery and discuss with the team about which drugs to hold on the day of surgery.
Total knee replacement leads to an average blood loss of about 1,000 ccs. The surgery involves cutting bone where there are active bleeding ends, and thus significant blood loss is incurred. Surgeons use various strategies to decrease blood loss during surgery. The techniques include thorough coagulation, IV medications to prevent blood loss, using plugs to block the femoral canal. Still, there is a significant patient population who will need a blood transfusion in the period after surgery. Bilateral knee replacement patients presently would need a blood transfusion and ask your treating surgeon what your preferences are.
Blood transfusion could be autologous (collected from the patient herself before surgery) or homologous (from another individual from the blood bank). The modern blood bank practices are very safe, and the chances of contracting a disease like HIV is 1 in 2,000,000, Hepatitis B is 1 in 2,00,000, and Hepatitis C is 1 in 1,390,000. The chances of contracting syphilis are almost nil. There is still the possibility of unknown diseases and allergic reactions after a blood transfusion. The medical team would inform you of all the risks and consent obtained for blood transfusion.
We have a unique protocol where we optimize your blood parameters before surgery and thereby minimize the need for blood transfusion esp. after a single knee replacement.
The total knee replacement involves placing the prosthesis in the most optimum position to reproduce the native knee joint function. There are a large number of techniques, prosthetic designs, and order of procedure followed to achieve this objective. This is not an exhaustive description, but only an attempt to highlight the current thinking in joint replacement in a simple language.
The incision to perform TKA is a midline approach where the skin is cut in the front of the knee joint and the joint approached. Below the knee joint is the “Extensor Mechanism,” which is the quadriceps tendon, patella, and the patellar tendon. Most surgeons use a standard medial parapatellar approach where the extensor mechanism is cut, and the knee cap turned outside and surgery performed. There have been variations that have been tried to avoid cutting the entire extensor mechanism like sub-vastus, mid-vastus, and tri vector approach. All these names are just an attempt to avoid cutting through the tendinous portion of the extensor mechanism, thereby improve rehabilitation. In the long term, none of this has been found to make a difference in the total knee outcome.

We named it as such because, in the scientific literature, there is a debate of either one the techniques, implant design, or rationale is better than the other. The discussions are of philosophical differences between two options. But sometimes we have seen that patients get worried if the surgeon is doing the right thing by opting for one versus the other. We intend to clarify doubts but base final decision after discussion with your surgeon.
These are two broad philosophies that evolved at the beginning of Total knee designs in the late 1970s. Some surgeons followed a measured resection where they measure the amount of bone and cartilage that is removed. Gap balancing technique uses soft tissue tension to guide surgical decision making after the first bone cut. Presently, most surgeons use a combination of this approach so that both the principles are used to achieve a good outcome
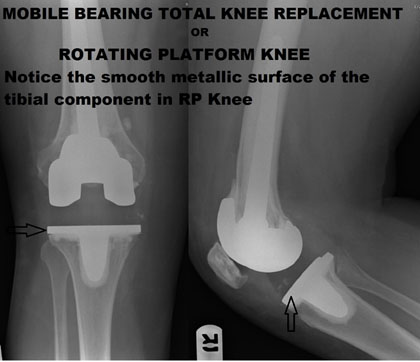
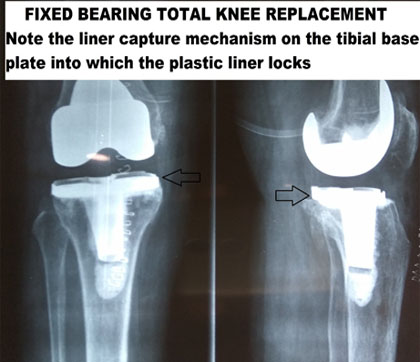
The plastic liner of the tibial surface either locks onto the metallic base plate or rotates on the plate. If locked on the plate, it is fixed bearing, and if rotating on the plate it is a rotating platform knee.
When the plastic component is locked, the movement happens only between the femoral component and the plastic liner. In the mobile-bearing TKA the liner conforms in shape to the femoral component distributing the stress onto a larger surface of the plastic component.
There is no difference in survivorship of both the prosthesis as long as it is done well, technically. Both the designs have been used extensively across the world, and surgeons have been happy with both of them. The primary determinant of the prosthesis is the surgical training and comfort level of a surgeon in that particular philosophy.
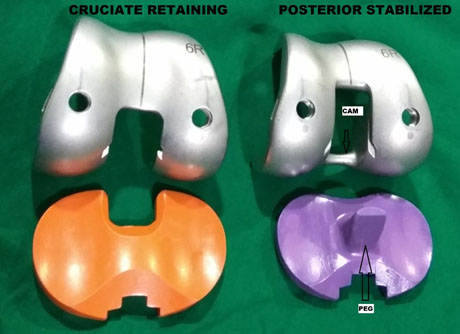
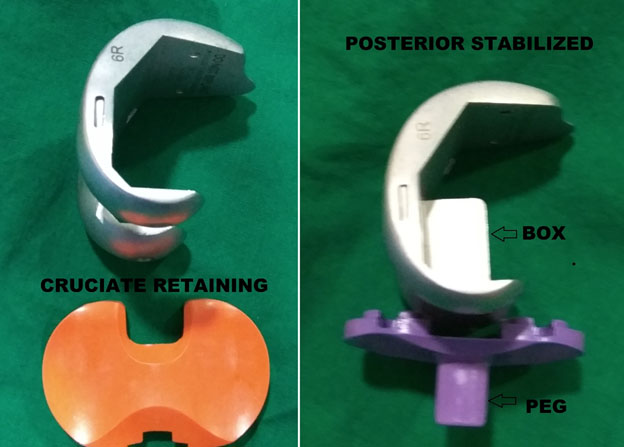
CR Vs. PS debate is an age-old debate in knee joint replacement with some surgeons retaining the Posterior Cruciate Ligament (PCL). PCL is a central ligament that stabilizes the knee joint. In OA knee, PCL is less damaged than the Anterior Cruciate Ligament (ACL). So, the long-standing philosophical debate has been that a PCL can be retained along with a significant amount of bone around its attachment. PCL sacrificing design helps the surgeon to replace the ligament function by the implant design change. 20-year comparison studies have shown no difference in the clinical outcomes.
The advantages of CR knee gives better proprioception while PS knee gives an option to correct deformities, which sometimes might not be possible with CR knee. The bottom line is, with good surgical technique, both designs give good results. A small section of surgeons in the western world are experimenting in retaining both the cruciate ligaments called Bicruciate TKA. But this is still not mainstream and is mentioned only to clarify that very few surgeons in India practice bi-cruciate TKA.
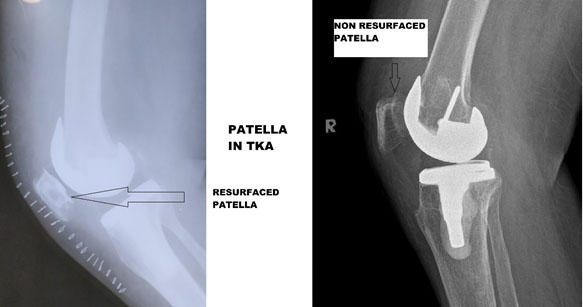
This has been another hotly debated topic among joint replacement surgeons should we replace the knee cap or not. The group who do not replace the knee cap believe that it does not contribute significantly to the arthritis pain. Results also show that patients who have undergone a TKA without knee cap replacement still do well. The reason for this big debate is that 15-20% of patients after TKA are not satisfied after TKA, and one of the common contributing factors is the anterior knee pain. Patients who have knee cap replaced after TKA have less chance of anterior knee pain than those who have not. But, it is only one of the factors for anterior knee pain
The downside of knee cap replacement is it weakens the bony bed on which the patella plastic component is fixed. The revision rate in patients who have undergone knee cap surgery is higher than those who do not have the knee cap replaced. The decision to replace the knee cap is individualized, and surgeons decide on case on case basis.
Total knee replacement is a satisfying surgery which gives a tremendous improvement in the quality of life for patients who are suffering from arthritis. But, it could also sometimes lead to some severe life-threatening complications and some troublesome complications.
Anesthesia has evolved over the last century and is considered safe in most patients. There is an element of risk involved when a patient is given anesthesia , which may include death, stroke, and spinal cord damage leading to paralysis or muscle weakness. Each of these complications is rare, but unfortunately, the percentage is not zero. After anesthesia, the commoner complications are soreness of throat, mild headache, drowsiness, discomfort, & urinary disturbances, which need simple appropriate interventions.
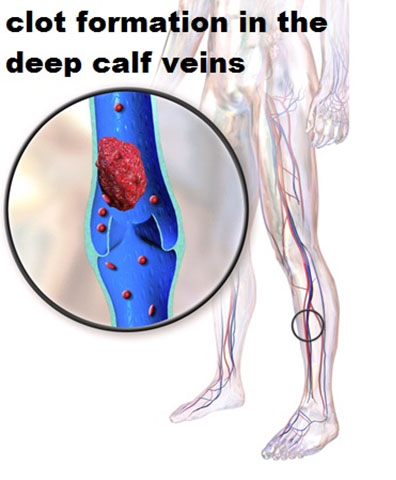
DVT is a widespread complication after Total knee replacement. It essentially is clot formation in the veins of the leg and thigh. There are contributing factors like age, previous history of clot formation, smoking, contraceptive pills, obesity, & pregnancy.
The problem of a clot in the legs could be local or general. If they block the veins entirely, it can lead to chronic swelling of the leg and pain. If the thrombus breaks free, it could block the vessels in the lungs and is called Pulmonary Embolism(PE). Pulmonary Embolism could be life-threatening in a matter of hours. The fundamental aim of preventive treatment after total knee arthroplasty is to decrease the incidence of Pulmonary Embolism by reducing the incidence of deep vein thrombosis.
There are minimal clinical symptoms of DVT like swelling, pain in the calf, and unfortunately, these are neither specific nor sensitive to make a clinical diagnosis. The primary diagnostics test employed will be Ultrasound to look for clots.
There is conflicting evidence about the true incidence of DVT in the Indian population. It has been quoted to be minimal to almost equal to that of the western people. Irrespective, medications are prescribed, and mechanical methods employed to prevent clot formation after TKA. Your doctor might prescribe low molecular weight Heparin, warfarin, or Aspirin for DVT prevention. You will have to take it after discharge based on your surgeon’s recommendation.
It might appear as a scary proposition to hear about death during an elective surgery like Total knee replacement, but unfortunately, it is not unheard. The incidence has been about 1 in 400-500 in the first 30 days after total knee replacement.
The genuinely devastating complication after a joint replacement is an infection. The incidence of deep infection after total knee replacements ranges from 0.5-2.0%. The problem with infection after a joint replacement are multiple. Except in the early knee infection most often than not, the entire prosthesis has to be removed. High doses of antibiotics are applied in cement in the knee joint as well as through IV medications. Finally, repeat surgery is performed. Essentially, what it means is that the cost of care after joint replacement infection would increase by about a factor of three, and the satisfaction decreases significantly in comparison to a successful outcome.

Surgeons employ a variety of preventive strategies to decrease the chance of infection during a total knee replacement. Techniques include Laminar airflow in the operating room, Pre-operative appropriate antibiotic usage, Special surgical suits inside the OT to decrease the chance of infection, usage of antibiotics in the cement (glue which helps to fix metal to bone) and pre-operative screening of the patients to prevent infection. Please talk to your surgeon about the necessary infrastructure at the institution and also infection prevention strategies to help avoid this dreaded complication.
There is a 0.2% chance that one can sustain a stroke after total knee replacement. There is a possibility of particular nerve dysfunction like peroneal nerve (which causes foot drop) due to a knock knee deformity present before the joint replacement surgery. Lower spinal cord damage (infrequent, but due to spinal and Epidural anesthesia) or femoral nerve damage due to the injection of drugs around the nerves is reported in the literature.
Knee stiffness can happen in some patients after a joint replacement irrespective of the surgical technique employed. This occurs in the immediate post-operative period. It is usually unrelated to the surgical procedure, and more due to genetic and post-operative adhesions in spite of adequate physical therapy. The knee joint needs to be loosened by manipulating under anesthesia to make the joint supple typically by around six weeks after surgery.
Numbness in the area of the scar is a widespread complication. Many times it is not right to list it as complication as it is almost universally seen to some degree. The incision cuts through the nerves, thus causing numbness. It could be troublesome if it forms a “neuroma” or a nerve swelling around the incision. Rarely, does numbness needs to be treated and it is a problem in a tiny percentage of patients when injections around that area can relieve the symptoms
Extra bone formation is sometimes seen around a knee replacement. It is not as common or clinically significant as after hip replacement. This problem is called “Heterotopic Ossification,” and only rarely surgically removed.
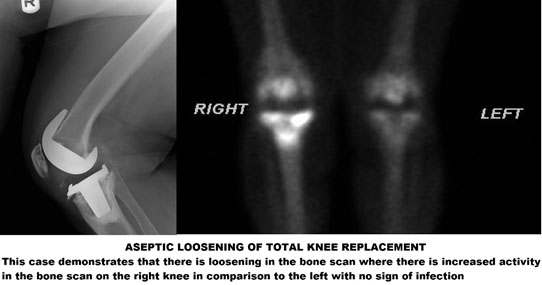
Some long term problems are inherent to joint replacement surgery. They are a late infection, loosening of the components, wearing of the bearing surfaces and fractures around the implants
Aseptic loosening is a situation where the total knee prosthesis loosens from the fixation with bone. It could be due to multiple reasons.Mal-alignment during surgery (where there is inappropriate distribution of pressure on the implant), Wearing out of the plastic liner and the plastic particles cause inflammation in the knee joint and thus causing loosening of the implant. The treatment options for Aseptic loosening is repeating surgery with removal of the loosened component and re-fixation with a different implant.
Amputation is a devastating complication, which happens in about 1in 6,000 patients. The need for amputation may be due to a blood vessel damage during surgery, stretching of the vessel after straightening of the knee if the patient had a long-standing deformity or due to persistent infection where every effort to eradicate infection has failed.