Book Appointment
Fillup the form to make an appointment with the doctor
Hip Problems Revision Total Hip Replacement
Disarticulation is a desperate attempt to save the life when every other method to salvage the limb fails. It is a morbid and disabling surgery and is used as a procedure of desperation.
Here is an example of a 65-year-old patient who had a bipolar hip prosthesis with massive infection, not responding to repeated debridement. She ultimately responded to hip disarticulation.
A fracture occurring at either the femoral stem or acetabular component is a peri-prosthetic fracture. Component stability and level of fracture decide the treatment option. The split either could be intra-operative during the primary surgery itself or could happen later due to trauma.

Acetabular fracture is of relatively rare occurrence. It can happen during a hip replacement when the surgeon will decide either to add screws or change to a slightly different cup design to fix the problem.
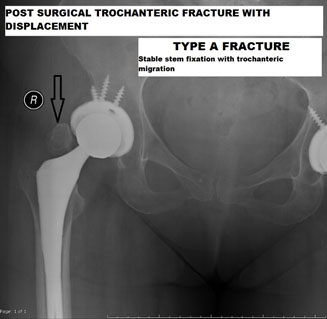
The femur fractures are more common either during the surgery esp. with the un-cemented component where the rates can go up to 5% while cemented hips have a low incidence of fractures. Postoperatively also, the rates of the un-cemented femur have a higher risk of fracture. The treatment of the fractures is dictated by a simple classification system called Vancouver classification
Type A- proximal metaphysis/ usually stable fractures. No need for major revision and a simple additional surgery suffices.
Type B- diaphyseal fracture or at the stem and bone, interface- could be stable where only observation or if unstable use a longer stem
Type C- occurs away from the stem tip. Most often than not, these patients require extensive revision surgery.
A male patient who underwent THR 2 years ago comes with pain in the hip, and X-ray shows this trochanteric fracture. Fracture treated with surgical fixation of the trochanteric fracture.
A 66-year-old male sustained an injury after a trivial fall presented with an unstable fracture and inability to bear weight. Revision performed with a long stem, and immediate mobilization was possible.



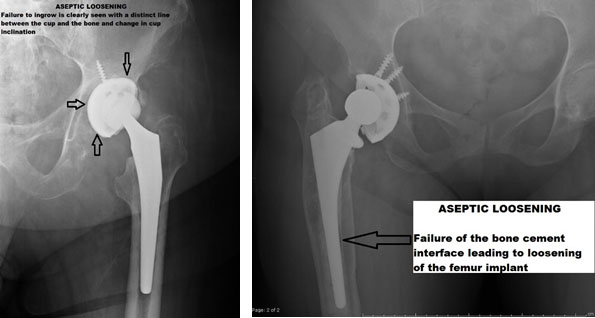
It is an inflammatory process where there is a loosening of the implant-bone interface leading to symptoms and reduction in quality of life. It usually is a long-term phenomenon and progresses gradually.
The prosthesis micro motion sets in a cascade of events that eventually leads to the destruction of the bone and implant interface. It is mediated by inflammatory cells in the human body called macrophages that cause progressive loosening. With less than 20 microns of micromotion, bony integration happens. While greater micromotion of around 150 micron leads to fibrous tissue and loosening.
The older generation of Polyethylene( Plastic liner between the metallic cup and the head) had a higher risk of wear(generation of particles). The microscopic plastic particles provoke inflammation
Patients usually have a well-fixed stem and lead to a progressive increase in the thigh and groin pain, which is worse with activity. The examination often reveals pain on rotation of the hip joint.
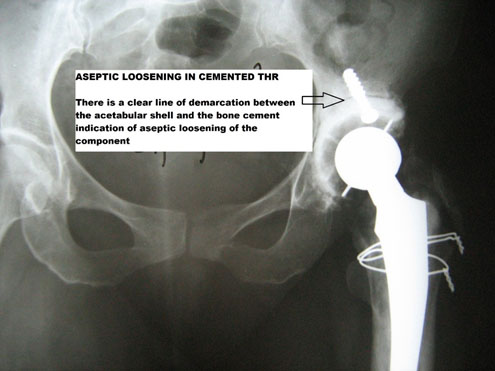
X rays usually demonstrate a clear line between the un-cemented cup, femoral stem, and bone, as shown in the following examples. Aseptic loosening can also be seen in cemented THR, where there will be a clear line demarcating cement bone interface.
The principle in cemented loosening is slightly different.Here, the particles generated by friction between the head of the femur and the acetabular component penetrates the area between the cemented shell and bone, leading to progressive loosening of the interface.
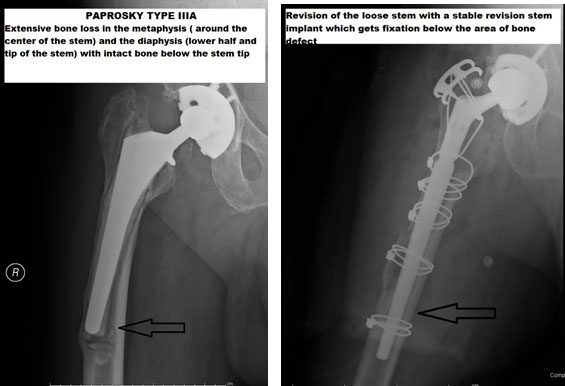
The principles of management of a loose total hip replacement are based on the component, which is loose, the available bone stock, and the presence or absence of infection. Eventually, the aim is for stable fixation of the implants. The bone stock availability determines the outcome and also the cost of surgery. Many patients are confused with the surgical costing of various centers and implant choices. The available bone is classified based on a system of classification by Dr. Paprosky both on the thighbone (Femoral) side and the cup (acetabular side). In general, the lesser bone stock available greater the sizes of implant and thus higher the cost of surgery. Several revisions in the past mean smaller bone stock available for further procedures.
1. Infection- 5%
Dislocation-5-10%
Limb Length Discrepancy
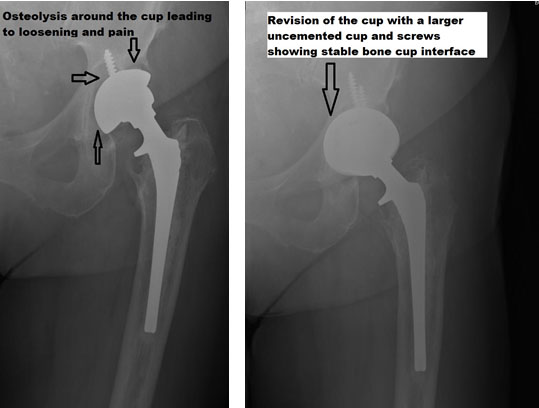
A patient who underwent THR 15 years ago presents with pain in the left hip. X rays showed osteolysis or breakdown of bone around the cup, which was worked up for infection and ruled out by blood tests. The patient underwent a successful revision hip surgery with implantation of a 3D ingrowth surface cup.
CASE EXAMPLE
A 65-year-old male had a total hip replacement performed about ten years ago presented with progressive pain in the thigh and difficulty to walk. The X-ray revealed an extensive loss of bone in the shaft of the femur. Extensive bone loss in the upper part of the femur (Metaphysis) necessitates the usage of an implant into the shaft of femur. Surgery with the long stem was performed and fixation obtained below the area of bone weakness.
Dislocation is one of the common causes for revision and technically challenging. Dislocation in more than 60% of times happen in the first month after THR.
Patient usually present acutely with severe onset of pain in the hip and inability to bear weight. Rarely in mal-positioned components, there can be subtle unrecognized instability.The activities that can provoke dislocation are trying to tie shoelaces, squatting in a toilet or pivoting awkwardly on an operated hip.
X rays will obviously demonstrate a dislocation in a THR.
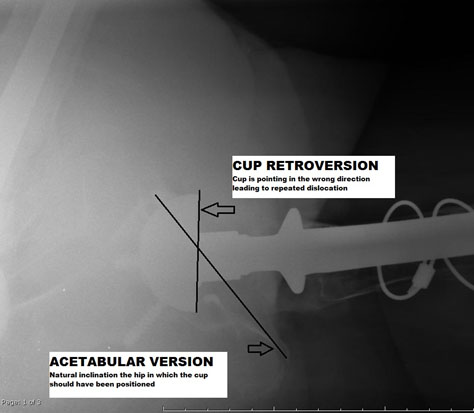
CT scanning is necessary to assess for implant malposition
The algorithm presented below is an useful approach in the management of dislocated hip.
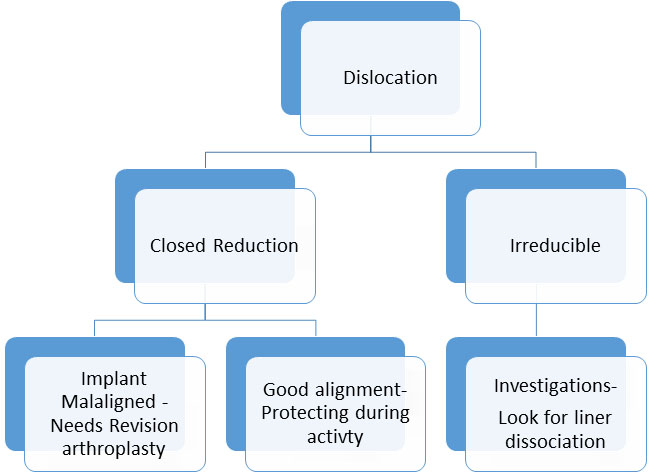
The principles of surgical treatment of dislocation is based on the underlying problem. There are some studies which demonstrate that posterior approach and smaller femoral head size (28 and 32mm) have a higher risk of dislocation.
| Implant malposition | Revision total hip replacement |
| Absent soft tissue envelop or repeated dislocation | Constrained THR/ Dual mobility THR |
| Underlying neurological condition | Converting to bipolar prosthesis |
Patient underwent THR for a long-standing childhood hip abnormality. 28mm head size was a risk factor in this patient ( most adults we use either 32 or 36mm head), and we had to use the posterior approach during the surgery. This patient had good component alignment so this patient was treated with closed reduction of skin traction-, which settled his problem in 4 weeks.
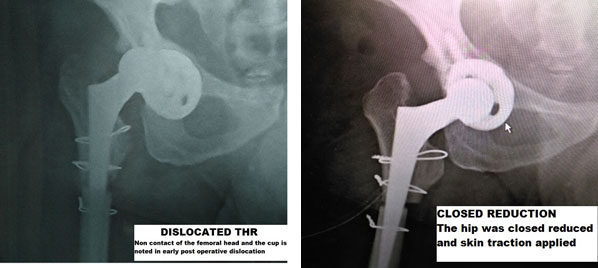
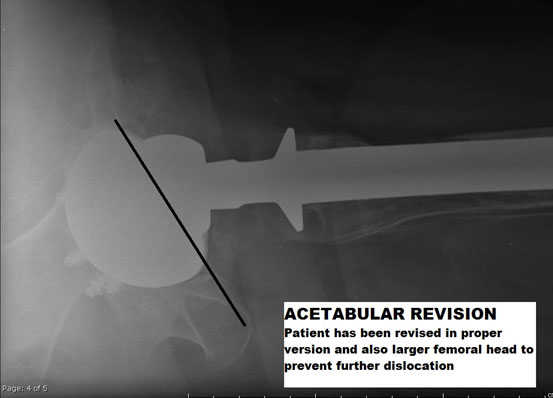
A patient who underwent THR a few years ago presented with dislocation, which had failed after repeated closed reductions. Component analysis displayed a mal-positioned cup, which needed revision hip replacement. We planned to increase the size of the femoral head to reduce further dislocation risk, and thus, we revised the femoral stem as well.
To reduce the risk of complications we use a unique approach in THR. At IORI we use lateral or anterior approach for all our primary hip replacements. It reduces dislocation risk and then we use implants that can accommodate a large head to reduce the risk further. Our infection rates are reduced by strict adherence to infection protocols and we use cemented prosthesis when appropriate to reduce the risk of perioperative fractures. The clear understanding and decision making algorithm of THR helps us to deliver quality care at a reasonable cost.