Book Appointment
Fillup the form to make an appointment with the doctor
Total Knee Replacement Revision Knee Replacement
The idea of needing another surgery after a knee replacement can be daunting. There are many reasons an individual might need a revision knee replacement. The questions from patients are always outcomes, quality of life, and pricing. Revision knee replacements, unfortunately, are expensive. The results are not as good as the primary knee, and usually, they make patients functional but do not restore the quality of life like a primary replacement.
Commonly, the reasons for revision of knee joint replacement is
Infection
Plastic wear out
Loosening of the component
Fracture
Ligament Imbalance
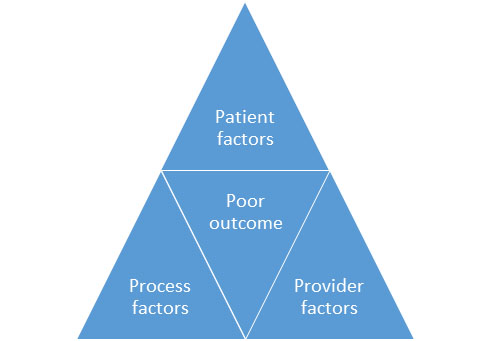
Infection is the most dreaded complication after joint replacement surgery. The incidence of infection has reached 1-1.5 % with improvement in techniques, and further reduction looks less likely given the medical problems in our patient population. The factors that determine the outcome are mentioned below.
If a patient has Anaemia, Diabetes Mellitus, Renal failure, or immunosuppression, they are at a higher risk for infection. Some of the patient factors are preventable, but some are inherent to the situation. The preventable risk factors for infection after a hip replacement is a pre-surgical correction of anemia and reasonable diabetic control.
The provider factors that contribute to the infection are the general operative environment and adherence to joint replacement protocol in the operating room.
Revision knee surgeries have a higher chance of infection than primary joint replacement.
Infection, if diagnosed within 2-3 weeks of symptoms, is an acute prosthetic joint infection, and if the patient has symptoms more than three weeks, then it is a chronic infection.
There is transient bacteremia (bugs are thrown into the blood during a daily activity like brushing the teeth and straining during toilet activity) that can reside on implants and cause infection. If acute, then potentially hospital and intra-operative contamination is a real possibility.
The symptoms of infection in a knee replacement are sudden onset of Pain, swelling, and discharge from a well-functioning replaced joint. The patient could also experience fever, chills, and difficulty to bear weight.
If a patient has a well-functioning replaced joint, any new onset symptoms are cause for concern, and the individual should seek medical attention as soon as possible.
Your surgeon will order a panel of blood tests, X rays, and admit if necessary. The earliest changes are in the inflammatory markers in the blood, and later on, radiological changes appear.
Your surgeon might aspirate (drawing fluid out of the knee) and send for further analysis. The tests performed on the synovial fluid will give useful information regarding the presence or absence of infection.
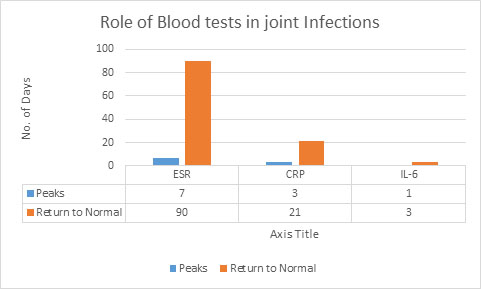
ESR (Erythrocyte Sedimentation Rate), CRP (C – reactive protein), and IL-6. Blood tests have a significant role in the diagnosis of joint infections. IL-6 is not widely available but drops rapidly once the infection is eradicated. CRP is widely used, and it becomes normal in 3 weeks, while ESR takes three months to return to normal. Reducing trend of inflammatory markers is reassuring for the eradication of infection
X rays can demonstrate evidence of bone damage, but X rays are poor indicators of infection.
Infection in the replaced joint can be either early or late. If infection occurs in the post-operative period of 4-8 weeks, then we call it an early infection. The common causes of early infection is either intra-operative or peri-operative. Intraoperative infection is where contaminants on the skin of the patient or from the immediate environment have entered the joint. Peri-operative infection is in the immediate period after surgery blood seeding of the joint with organisms. Late infections- occur about six months after joint replacement are all virtually bloodstream based infections. Many daily activities like brushing teeth, straining when constipated can lead to transient bacteremia (bacteria getting into the bloodstream). Most often, transient bactermia is handled by the patient’s immune system. If due to either lack of immunity or excessive bacterial load body is unable to take care of these organisms, then replaced joints get infected.
Infection is more common in patients who have Rheumatoid Arthritis, Chronic Renal failure, or Diabetes Mellitus, as in all these conditions, patients have low immunity.
Patients generally tend to have symptoms if a replaced joint is infected. The signs could be local like increased Pain, swelling, decreased range of motion & warmth or systemic symptoms like fever, loss of appetite, decreased functional ability. If there is a discharge (pus or unhealthy fluid), then the joint is usually infected.
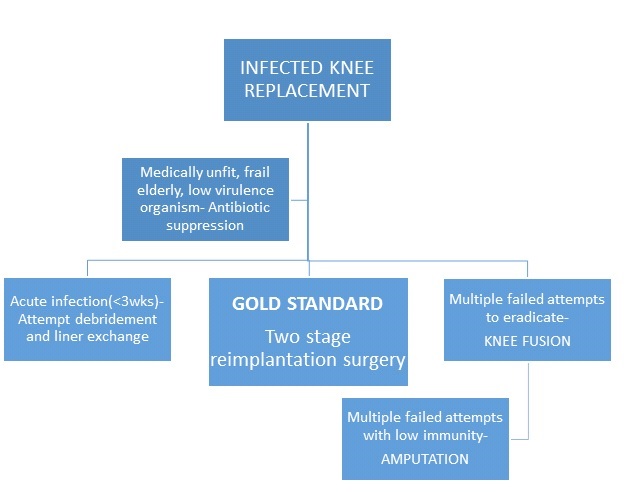
The treatment for a replaced knee infection is mostly surgical. The available treatment options are shown in the table below.
| TECHNIQUE | METHOD | ADVANTAGES | DISADVANTAGES |
|---|---|---|---|
| Chronic suppressive antibiotic therapy | Only IV or oral antibiotic is given | No surgery and associated medical risk 10-15% success rate | Little success and can progress to sepsis |
| Liner exchange and Debridement | The implant component is retained, but the plastic liner changed | Useful in acute infection Less extensive surgery and less expensive | 50-55% success rate Depends on the type of organism for an outcome |
| Single-stage re-implantation | Surgery where all the implants are removed, debrided and new set of implants inserted | One surgery solves the problem Eradicates the biofilm and better than just liner exchange Lower cost with good functional outcome | 80% success rate Higher risk of residual organisms and thereby infection flare |
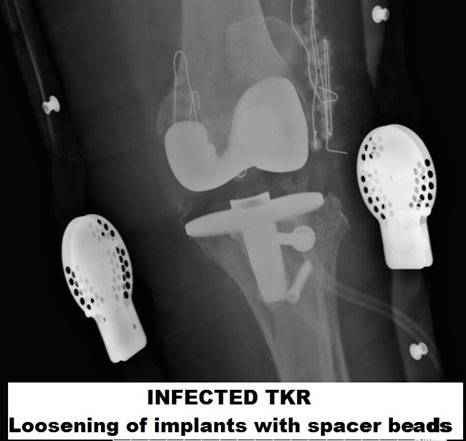
| Two-stage re-implantation | Surgery where implants are removed and spacer inserted The second stage after six weeks where a new set of implants are inserted | The highest chance of infection eradication Can monitor for infection eradication and time the revision surgery | 90% success rate Two surgeries and risk of two anesthesia More expensive and patient morbidity during six weeks of the spacer with limited mobility |
| Excision Arthroplasty | All the implants are removed and patient is left with unstable knee | Infection eradication is effective Less expensive and a single surgery sorts out a problem | Success rate of 70-90% Unstable knee will limit the mobility of the patient and make them wheelchair-bound |
| Knee fusion | The implants are removed fully | The thigh bone(Femur) and tibia( leg bone) are fused and make for a stable platform to walk on | The success rate of around 80% Proper gait but difficulty to sit as there is no knee bending |
| Amputation | The limb itself is removed | The lifesaving situation with a highly toxic organism Indicated when there is bad skin, no soft tissue cover | Success rate higher but very morbid and the patient is functionally limited |
A 60-year-old male had an infection in the knee joint which was planned for a two-stage revision but underwent an articulating spacer- mostly maintaining the ability to bend the knee. The patient was comfortable until the final revision, as the patient was able to bend the knee until three months when he underwent the last revision surgery.
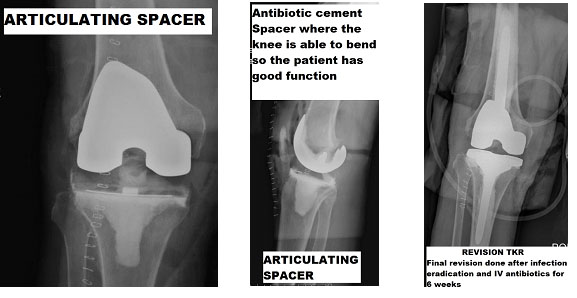
A patient underwent TKR, after which she developed an infection in the knee joint. Her knee was aspirated, and acute Staphylococcal infection was confirmed. She was treated with a standard static cement spacer. The spacer had high doses of antibiotics, but where there is no ability to bend the knee and got six weeks of IV antibiotic. At the end of six weeks, she underwent a final revision knee surgery and was operated with a revision knee replacement.

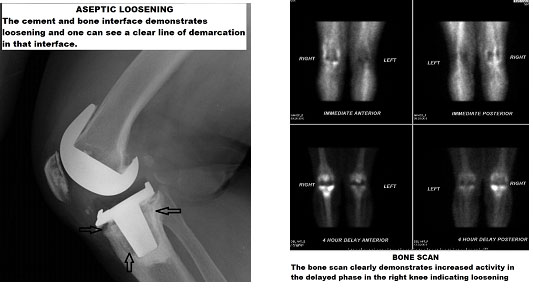
Aseptic loosening is a condition where there is a progressive loosening of the implant from the bone without any evidence of infection. Primarily, because of the inflammation induced by the small plastic particles from the liner (the plastic insert between the metallic components)
Patients usually present with startup pain (Pain when they start walking) and progressive worsening of quality of life.
X rays are usually enough to demonstrate loosening of implants, but in, some situations the patients might need to undergo bone scans to diagnose subtle loosening.