Book Appointment
Fillup the form to make an appointment with the doctor
Health Professionals DEVELOPMENTAL DYSPLASIA OF THE HIP
METATAG- hip clicks and clunks, Ultrasound of the hip, Pavlik harness, double diaper technique, hip osteotomy, open reduction of the hips, Closed reduction of the hip and spica application. DDH is a fascinating disorder with a range of hip pathologies, which might range from a mild uncovering of the head of the femur to the complete dislocation of the hip joint presenting at birth. Previously this disorder was called Congenital Dislocation of the Hip. Teratological dislocations are conditions where the primary pathology is Arthrogryposis, Myelomeningocele, or Larsen’s syndrome.
The incidence of the dislocated hip is 1 in 1000, and Dysplastic hip is 1 in 100, which essentially means that dysplastic hips are ten times more common than dislocated hips. 5 F’s of DDH- It is more common in the Firstborn, Female, Foot First (Breech Presentation), Family History & Fluid Deficit (Oligohydramnios) Associated conditions- Many “Packaging Deformity,” which are disorders that occur due to tight uterine and abdominal musculature.
The DDH examination in the newborn consists primarily of two provocative tests. Barlow and Ortolani tests. These tests are useful till the child is of 3 months of age. The feeling one gets on performing these tests is called CLUNKS rather than CLICKS, which can be safely ignored as they are relatively common. ORtolani (Outside Hip is Reduced) – the pressure is applied by the index and middle finger of the examiner on the trochanter to push the hip forward by elevation and Abduction of the flexed femur.
Barlow- dislocates a dislocatable hip by adduction and depression of a 90 degree flexed femur.
There are contractures of the soft tissue, and thus the provocative tests cannot be employed. The most sensitive test is the limitation of Abduction if unilateral or in bilateral cases both the hips have weakness in the Abduction
There is a limb length discrepancy when the knee is flexed to 90 degrees and hips to 45 degrees. Galeazzi sign is significant in a dislocated hip where there is a shortening of the affected side.
There is pelvic tilt due to shortening of the extremity as well as equinus gait, and plantarflexed position of the foot as compensation for shortening Lumbar lordosis- which is a compensatory increase in the spinal curvature due to the posterior position of the hip center as well as the contractures that develop Waddling or Trendelenburg gait- Kids tend to walk like a full-term pregnant woman due to hip abductor insufficiency

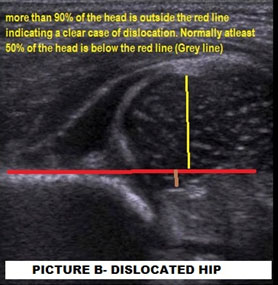
USG is an essential investigation before the ossification of the femoral head, which happens at the age of 4-6 months. It is investigator dependent. An experienced operator needs to perform as “a normal hip might be made to look abnormal, and an abnormal hip cannot be made to look normal.” It helps to see the acetabular bony anatomy, femoral head, labrum (which is the lining of the mouth of the acetabulum), and the hip capsule. If done within 4-6 weeks of birth might increase the number of false positives- so ideal time to obtain a USG hip in a questionable hip is 4-6 weeks after birth. It is not cost-effective for routine screening of patients. It is useful in monitoring of reduction of a hip after Pavlik Harness usage
Two numbers to remember is- an Alpha angle, which should be more than 60 degrees, and coverage should be more than 50%.
Plain X rays are helpful after the age of 4-6 months when there is ossification of the femoral head physis. Two entities need to be understood- hip dislocation and hip dysplasia. No contact between the femoral head and the acetabular cartilage is a dislocation of the hip. Partial contact between the femoral head and acetabular cartilage but not adequate is hip dysplasia.
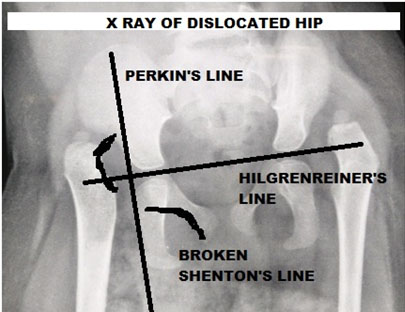
As shown in the X-ray, the femoral head should be typically in the lower inner quadrant while in a dislocated hip, it is in the upper outer quadrant. The horizontal line that connects the two triradiate cartilage is called Hilgenreiner’s line. The vertical line on the outer margin of the acetabulum that is perpendicular to the above line is called Perkin’s line. There is also a break in Shenton’s line.
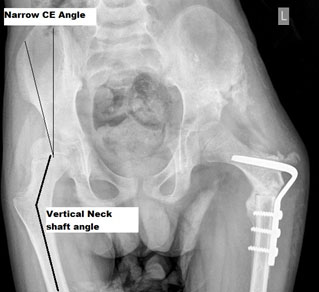
It is an entity where there is no adequate lateral and anterior coverage of the hip joint. Dysplasia is measured radiologically by certain angles in the hip joint. It is assessed by taking AP and false profile view of the affected joint. Acetabular index- It is useful after six months of age and is generally less than 25 degrees. It is an angle formed by the triradiate cartilage and the lateral point on the acetabulum. The center-edge (CE) angle of Weiberg – The angle formed by a vertical line from the center of the femoral head with another from the center to the outer margin of the acetabulum.
Generally, all reducible hip are treated with a Pavlik Harness. It’s usage requires a well-functioning musculature. Pavlik harness cannot be used in teratological hips.
Closed Reduction and Spica Casting (POP) of the lower extremities or if there is a failure of Pavlik harness

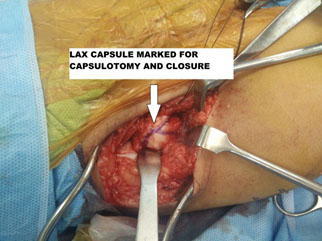
pen reduction along with necessary bony surgeries either on the pelvic or the femoral side as appropriate.
Common Problems encountered by pediatricians during the treatment of DDH
The role of the Pavlik Harness is to keep the hips flexed to 90-100 degrees and Abduction to 50 degrees. Given the rapid growth of a child, sometimes, the harness needs to be changed every 3-4 weeks. Once a baby is placed in the harness and is well-fitting, then kids are comfortable in the harness, and other causes should be ruled out.
The Anterior Strap should be at the level of the nipple. The hip should be flexed to about 90-100 degree Hip to be abducted to 50 degrees and not more. Should not be able to bring the legs to midline. The child should be kicking her legs freely- if not it could be a sign of femoral nerve palsy and needs immediate orthopedic review. Parents should not remove the harness and only change diapers and clothing below the harness.
Any child who has been treated with a hip spica can have constipation due to various post-surgical factors like pain, opioid medication as a cause of constipation. Please discuss with the treating surgeon before starting medications for constipation as soiled spica can cause severe damage to the skin and could result in deep ulcers in the buttocks.