Book Appointment
Fillup the form to make an appointment with the doctor
Hip Problems Complex Primary Total Hip Arthroplasty
Complex primary THR essentially means that the patient has a surgical problem that has all the complexities of revision joint replacement but is undergoing surgery for the first time. The approach for a patient with complex primary pathology is slightly different from the primary THR.
The implants necessary to perform complex primary THR are expensive and mostly organized before the planned surgery. The complications in these cases are serious, and the treating surgeon and the patient should discuss the same.
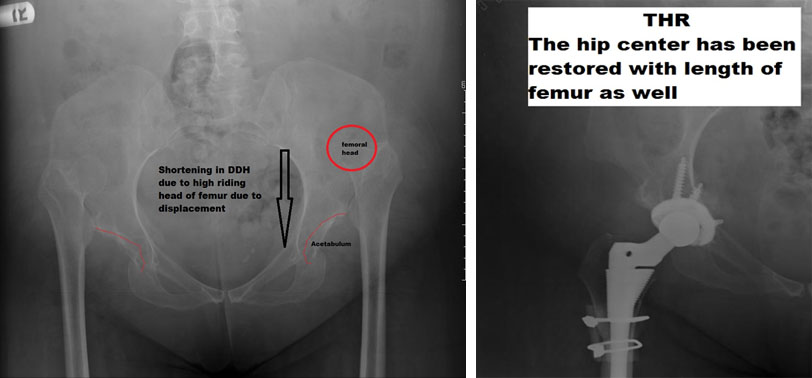
THR in a congenital dislocated hip is different from a post-traumatic dislocated hip and arthritis. In a congenitally dislocated hip, the patient is walking in the dislocated position for a long time, and the usual habitus of the patient is with an exaggerated spine curvature. In a traumatic situation, the joint surface usually is normal on the socket side (acetabular side).
DDH is a condition where the hip is congenitally or from an early age outside the pelvic socket piece.
A 35-year-old lady presented with pain deformity and difficulty to walk. Pain limited activity of daily living, and her Quality of life was affected by her symptoms.
A 58-year-old gentleman with an injury at the age of 18 years presented with significant hip pain and difficulty to walk. Investigations demonstrated that the patient had a dislocated hip and arthritis in the false joint. We performed a THR with the positioning of the cup in the original area and fixing the arthritic joint with the head of the femur.
This surgery required precise surgical planning with a preoperative CT scan, modification of the standard technique to preserve the head of the femur, thus enabling the fixation in the arthritic surface.


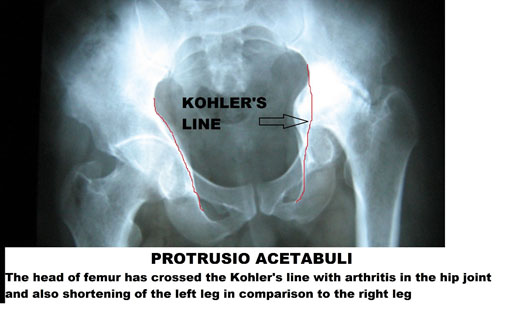
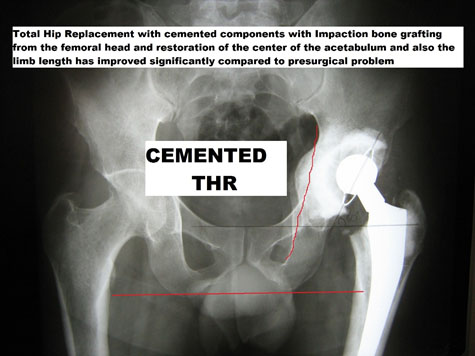
Protrusio is a clinical condition where the hip is seated deep and leads to arthritis in some situations. It is common in Rheumatoid arthritis, trauma, and certain genetic conditions like Osteogenesis Imperfecta and ankylosing spondylitis.
Radiologically, the head of femur crosses the Kohler’s line and that indicates that there is a weak inner wall of the acetabulum (socket piece of the hip). The treating team has to plan techniques to reinforce or reconstruct that wall before performing a total hip replacement. Otherwise, there can be a breach in the inner wall, and the cup can end up being placed inside the pelvis with damage to the bone.
The bone is generally osteoporotic (structurally weak). Dislocating the hip can be a challenge, needs implants that are used for revision surgery, and the cost of operation is higher due to longer operating hours, blood loss, and possible complications.
A 45-year-old man with functionally limiting hip arthritis for four years due to Rheumatoid arthritis presented with left hip pain. On evaluation, he was found to have a protrusio hip who underwent cemented THR with impaction bone grafting.
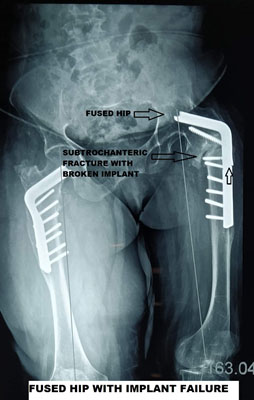
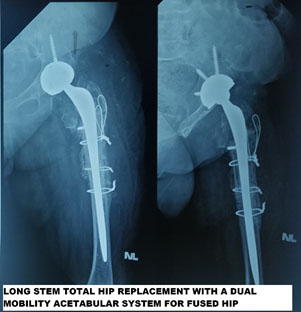
Patients who have fused hip for whatever reason tend to develop problems in the knees and spine with aging. Hip fusion puts stress on adjacent joints- it affects their gait, and their functional ability decreases rapidly with aging.
A 55-year-old woman who had bilateral hip osteotomy done 30 years ago presented with right knee pain and severe lower back pain. She was examined elsewhere and recommended for knee arthroplasty. On examination, she had pain and jog of movement in the left hip. The patient’s X-ray demonstrated failed hip implant, fracture of the femur, and a fused hip. The patient was treated with complex primary hip arthroplasty. Uncemented multi-hole acetabular cup for good fixation, Dual mobility cup to reduce the risk of dislocation, Long stem cemented stem for better fixation into the thigh bone and immediate weight-bearing ability.
Obese individuals have a higher complication rate after total hip replacement. Few of the problems of THR in obese individuals are as listed-
The role of bariatric surgery before total hip arthroplasty has been a topic of debate in the surgical community. The evidence regarding the role of bariatric surgery at best has been mixed; a meta-analysis published in the year 2016 in Bone and Joint Journal by smith et al. showed no reduction in complications rate with bariatric surgery for joint replacement. Individual studies have shown that there is some reduction in the complication rates. Common sense dictates that a patient should be counseled regarding the possibility of seeking bariatric surgery or weight loss before undertaking joint replacement surgery. There is significant evidence that obese patients generally tend to gain weight after joint replacement than lose weight.
The current surgical practice is that if an obese patient has significant arthritis limiting Quality of life with an inability to lose weight by exercise and diet, then joint replacement is offered. Whereas if the patient has mild to moderate symptoms and has exhausted all other methods to lose weight, then bariatric surgery precedes a joint replacement.