Book Appointment
Fillup the form to make an appointment with the doctor
Health Professionals Cerebral Palsy
Cerebral palsy (CP), by definition, is a “non-progressive Neurological condition due to an irreversible insult to the immature brain.” It is characterized by varying degrees of motor defects meaning lack of coordination, the strength of the muscles, tightness in the muscles, and gait abnormality. It occurs because there is an insult to that part of the brain which controls motor movement. There could be problems of vision, swallowing, and also many times, these children have poor intellectual prowess as well. It is not a homogenous clinical entity and can range from a subtle weakness in a muscle or a group of muscles to a wholly dependent and bedridden child.
One of the most common misconceptions about CP is all of it caused due to “Hypoxia” at birth. Even though it is a common cause, it is not the ONLY cause. The causes could range from genetic mutations, Infections in the mother or the child during pregnancy, Hypoxia (Lack of Oxygen during Birthing) or infection or head injury in a young child up to the age of two years.
| Maternal | Fetal | |
|---|---|---|
| Infections | Cytomegalovirus Rubella Syphilis Herpes Chickenpox Toxoplasmosis |
Viral meningitis Bacterial meningitis and Encephalitis |
| Toxins | Smoking and other drug abuse, Mercury exposure | |
| Complicated delivery, delayed second stage with instrumented delivery | Low birth weight, NICU admission at birth, Severe perinatal jaundice |
TABLE-1 RISK FACTORS IN CEREBRAL PALSY
Cerebral palsy manifests initially with delayed milestones and usually diagnosed at the age of 2 years. CP is classified commonly as-
Athetoid CP is a clinical entity where the child does not have control over the movements with significant involuntary movements. Ataxic CP is a situation where there is a lack of coordination, and the child will have difficulty with fine activities like eating or buttoning a shirt. In mixed CP, there are various elements, and the types of CP generally indicates which part of the developing mind has been injured. Most of the other forms of CP rarely come to the attention of orthopedic Surgeons and generally interventions in non-spastic CP kids can make life difficult Spastic CP- This is the most common form of CP. Spasticity is the tightness of the muscles and stiffness associated with it. Spasticity is a velocity-dependent increase in muscle tone. It could be HEMIPLEGIA, where only one side of the body is affected. DIPLEGIA, where both lower limbs are affected slightly more than the upper extremity. Finally, QUADRIPLEGIA where all the four limbs are affected
Management of CP is a multi-disciplinary approach, and patients must be aware of the process. The parents and caregivers must be open-minded and have a healthy discussion regarding the goals of managing a child in CP. Many parents and some caregivers stress too much on mobility, but the order of priority of CP management is always about communication, social development, and then mobility management.
In a country like India, with limited financial resources and CP affecting the more impoverished socioeconomic strata, the families must plan for resource rationalization. The treating team should clearly explain the treatment goals and realistic outcomes. The families weigh the benefits and proceed with treatment. Treating CP does not affect just the child but affects the entire family. Many CP parents are themselves in need of help either with their health (carrying a heavy CP child with back and other problems, emotional problems due to relationship stressors) or financial. They make tremendous sacrifices to provide for the unfortunate child.
There are various scoring systems designed in CP, but the most used and enduring has been the GMFCS grading (Gross Motor Function Classification System). It is a simple, useful classification helpful in communication as well as treatment planning with five grading system
Type 1 – walks without functional limitation
Type2 – Walks with functional limitation
Type3 – Walks with a handheld mobility aid
Type4 – Limited labored mobility with aids and needs motorized assistance for distances
Type5 – Wheelchair bound
| AGE | MOBILE ( GMFCS I-III) | NON-AMBULATORY (IV-V) |
|---|---|---|
| 0-5 Years | Spasticity management Orthotics | Spasticity management
Orthotics
Hip Surveillance |
| 6-18 | SEMLS ( Single Event Multi-Level Surgery) | Quality of life Management |
Spasticity, unfortunately, is an unrelenting accomplice in a CP patient’s life. Spasticity management consists of using intrathecal Baclofen ( rare to nonexistent practice currently in India), Oral baclofen, or Intramuscular Injections. Intramuscular injections could either be Botox or Absolute Alcohol. Botox is an expensive medication costing about 30,000 rupees at each sitting for injection, while absolute alcohol is a poorer alternative. Alcohol causes muscle and nerve degeneration with the possibility of worsening weakness. But, it is a cost-effective solution for unaffordable clinical situations.
Orthotics help in preventing deformities or maintaining corrections after surgery. They could consist almost universally like AFO (Ankle Foot Orthoses) or Hip Abduction Splints to prevent hip dislocations.
Orthopedic surgeries in cerebral palsy are done with certain fundamental principles in mind. Correction of multiple deformities in a single sitting (SEMLS)is the standard of care. Stable fixation, so that early mobilization is a possibility and quick return to activity with aggressive post-surgical physical therapy. SEMLS consists of trying to address hip, knee, and ankle problems in a single stage. It consists of selective tendon lengthening, transfers, osteotomies of bone, and fusion of bones and joints (arthrodesis).
It is critical that the CP child is objectively and thoroughly evaluated, but also a three-dimensional gait analysis helps in proper surgical planning of a CP child. It helps in analyzing individual components of deformities and planning the correction.
Here is a sample of gait analysis information which helps the treating surgeon to plan the surgical procedure. Gait is a complex co-ordinated event and is very difficult to assess visually for the complexity of treatment necessary. That is why gait analysis helps us to plan the surgery better.
It consists of lengthening select groups like the calf muscle (Only a component rather than the full tendon), Hamstring (back of the calf muscle), the adductors (inner thigh), or the iliopsoas (the hip bender) to prevent deformities at the hip, knee, and ankle. The critical point which a surgeon has to evaluate in tendon lengthening is the “adequate dosage.” If not done well, it can lead to reverse deformity or at worse, make a walking child immobile.

Some tendon groups in CP kids tend to overact and need a release, and some need to be supplemented. In a stiff knee child, the Overacting Rectus needs to be transferred to the hamstrings. Similarly, part of the tendons can be split in the feet and moved to the other muscles.

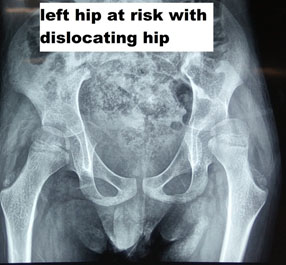
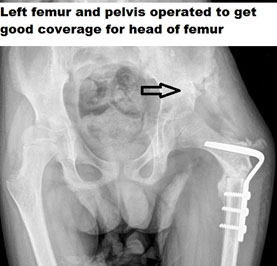
A large number of times, CP kids tend to develop bony abnormality due to deforming muscle forces. The kids are born with normal bony architecture, but as they grow old, muscle spasticity causes deformity. The deformity at the hip could be a subluxation, flat foot, or in-toeing and out-toeing at the feet. The assessment of CP is incomplete without an objective evaluation of the muscular and bony deformity. If there are already bony changes that have developed, and if only muscular procedures are done, then they are bound to fail. Bony correction must also be done simultaneously.
Bony procedures in CP could consist of Osteotomies like Varus Derotation Osteotomy of the hip (VDRO) if the head and neck of the femur are vertical. We might need to add a Pelvic Osteotomy to give appropriate coverage for the head of the femur. There could be a need for derotation osteotomy of the leg (tibia) or the thigh bone (femur) to ensure that the child can walk appropriately or in Bedridden kid’s toileting activity is done easily.
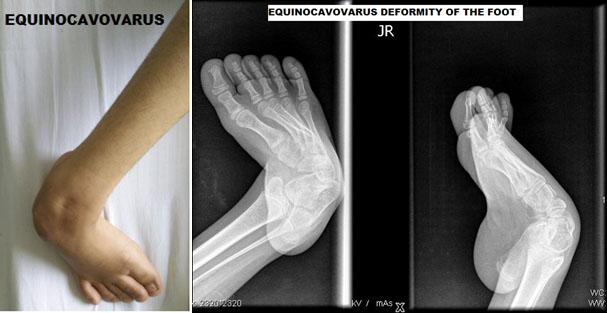
CP children commonly can have a deformity of the foot like a flat foot with overacting evertors and would need bony procedures to correct those deformities. The common foot deformities that present in the pediatric age group is
Equinus is a pervasive problem with kids with cerebral palsy. Overactivity in muscles that pull ankle down and lack of ability to lift it causes an imbalance leading to the development of equinus deformity. The management emphasis should mostly be on the prevention of this condition. It would consist of static splints at night, stretching exercises passively by the family. Is these measures do not work, then the patient needs either botox injection or surgical lengthening of the gastrosoleus complex.
Equnioplanovalgus is a reasonably common deformity in cerebral palsy. The child walks with pronation or more on the inner border of the foot with minimal contact on the outer edge leading to a bad flat foot and painful gait. The foot works like a tripod, and any malalignment leads to problems in gait. Firstly, orthotics are prescribed in mild deformity. Severe deformity necessitates calcaneal lengthening as well as soft tissue surgery to rebalance the muscular forces.



Cavovarus is of slightly lesser incidence, and it is there opposite of flat foot. In this condition, the foot is turned inside; the position is described as supination. The child walks on the outer border of the feet and develops callosities on the outer edge. If the child has a persistent pain because of this, then it would require a tendon transfer to balance the muscle forces. The tendon transfer is called “Split transfer of the tibialis posterior.”
This question has to be dealt with compassion and reality. In short, the answer is NO. The most important predictor for gait is the independent ability to sit at age two years. If a child does not walk by age seven years, the child will probably never ambulate.
Most hemiplegic kids will walk, diplegic kids will walk in up to 80-90% while quadriplegic kids gait ability is pretty variable from 10-60%
1. 15-60% of CP patients have a seizure disorder, and it is essential to ensure anti-seizure medications are adequate and absent seizure recognized.
2. A true confirmation of CP can only be done at 3-5 years of age when the brain is fully developed.
3. Speech, vision & language assessment and intervention by appropriate team members
If there is late sitting (after eight months)
Delay in walking- after 18 months
Asymmetric hand function (hand preference in less than a year old infant)
This is an important dilemma for pediatricians when they are deciding for a referral for CP surgery. In the Indian context majority of our patients will need a multidisciplinary approach for taking care.
Many times these kids need insertion of PEG tubes (Percutaneous Endoscopic Gastrostomy) tubes for which a laparoscopic/Paediatric surgeon is necessary
Appropriate techniques and intervention can improve the vast majority of orthopedic problems in CP. The “DOSING” of surgical treatment is extremely critical and needs to be dealt with appropriately. The treating surgeon must spend time analyzing the gait, formulate a plan, and assure the family about the goals of treatment. Many families have an unrealistic expectation, and surgery will improve the gait and quality of life but will not make the child normal. So, the treating orthopedic surgeon should understand the problem, and a new problem created by inappropriate surgery might sometimes make a child essentially nonambulatory.
A small subset of non-ambulatory CP (GMFCS V) might need permanent surgical intervention to treat spasticity. Selective Dorsal Rhizotomy (SDR) has been used to reduce spasticity and morbidity. These patients need to be referred to neurosurgeons, who are proficient in treating such patients.
Many parents out of anxiety, ignorance, and hope fail to plan for the rationing of resources for their CP kids. CP is common in the middle income to lower socioeconomic strata doctors, need to act as counselors regarding judicious resource utilization. The rule of thumb, which has to be followed, is always to see if a child can be made independent. The biggest misconception which families have is equating “Ambulation” with “Independent.” Pediatricians need to counsel families saying that language, communication, vocational training is more important than gait. Many families spend almost 1/3-1/4th of their total income on physical therapy, which is the least rewarding of all the interventions. Many parents and typically mothers can be taught to perform stretching exercises saving on the money that is spent on spasticity management and reallocate the resource for other needful utilization.
This is an essential question with long term implications. Hardly there is any need for orthopedic surgery in the less than 6-year-olds except when the hip is at risk. Most Orthopedic surgical interventions are around the 7-9 year age group so that there is adequate compensation for gait abnormalities.